***Hot topic/History Of Mental Health & The Black/African American Community***
The History of Psychiatric Diagnoses of Black/African American People.


Drapeto….what????? The History of Psychiatric Diagnoses of Black/African American People....
Before I begin, I would like to point out that this is not an APA written paper; however, I did cite much of what I presented here so that the readers can go back and review the full articles I reviewed for this piece. When I tell you that you are going to desire to learn more, trust me…this stuff is deep, too much to include here. Refer to the reference list, go back and take a look at some of these articles. If you don’t know, you can’t do better. #SANKOFA
Recently, my godbrother shared a post on Facebook that caught my attention. There was an image taken in 1851 of a White man by the name of Dr. Samuel Adolphus Cartwright. The image appeared to be a book cover of some sort titled, Drapetomania A Psychiatric Diagnosis: “Runaway Slave Syndrome”.Now, anyone who knows me knows that it was impossible for me to see this and continue to scroll without researching the Dr. Cartwright character and his “diagnosis”. To my surprise, I learned a lot about the history of mental health. Funny (not funny) thing is, when we (those studying in the field) begin our undergrad we take at least one course that reviews the history of psychology. I know that I do not have the greatest memory, but I can promise you that I have never heard of this guy and his diagnosis.
The first thing that struck me when I started researching Cartwright was the apology provided by the American Psychiatric Association (APA) in January of this year…like what?!?!?! I will not go into too much detail about the letter (check it out here), but I will tell you that APA is “beginning the process of making amends for both the direct and indirect acts of racism in psychiatry” (APA, 2021). The organization further admits that there were, “discriminatory and prejudicial actions within the APA and racist practices in psychiatric treatment of Black, Indigenous, and People of Color” (APA, 2021). Lastly, the organization admits that there is a connection “with larger social issues, such as race-based discrimination and racial injustice, that have furthered poverty along with other adverse outcomes” (APA, 2021).
Since the APA's inception, “practitioners have, at times, subjected persons of African descent and Indigenous people who suffered from mental illness to abusive treatment, experimentation, and victimization in the name of "scientific evidence," along with racialized theories. Similar, race-based discrepancies in care also exist in medical practice today” (APA, 2021).
Another thing that I learned, which I kind of already knew but did not have updated data on, is the alarming rate of suicide attempts amongst Black/African American youth. We must pay attention to this because this is huge!!! Between 1991 and 2017, suicide attempts among Black/African American youth increased by 73% while the number has decreased among White youth (Abrams, 2020). Lindsey, Sheftall, Xiao, and Joe (2019) conducted a study on 198,000 high school students confirming this to be the case. To add, Bridge, Horowitz, and Fontanella (2018) confirmed that there is an increased risk of suicide among Black/African American boys between the ages of five and 11. The issue has grown to a point where mental health providers are finally starting to recognize the suffering of the Black/African American community. Here we are in the 21st century, a time when equity still does not exist. In 2019, the Pursuing Equity in Mental Health Act was presented; in 2019! Unbelievable!
Moving along….







My reason for sharing this information is to show the connection between past trauma to present-day trauma. Over the years, we have heard a lot about posttraumatic stress disorder (PTSD) in the Black/African American community. We have been told that this is a disorder that, although it is experienced by all races, is generationally passed down in the Black/African American community. Through research, it has been determined that continued exposure to trauma, since enslavement, plays a role in the continued effects of PTSD (Sibrava, N. J., et al, 2019). Today, we will get an understanding of where this all begins, and I am not referring to enslavement in and of itself, but rather the psychological implications that have been burned into the minds and hearts of White people in this country. FYI, as I research, I am writing so this is all new news to me.
Back to Dr. Samuel Cartwright…
A 58-year-old psychologist and surgeon, Dr. Cartwright practiced in Louisiana, Alabama, and Mississippi. He held the position of chairman of the Louisiana State Medical Association committee. The group spearheaded the research on diseases that were specific to the “Black folks” as he mentioned in his annual convention report entitled, “A Report on the Diseases and Physical Peculiarities of the Negro Race” (PBS.org, nd).
(If you are interested, the PBS.org link in references is where you will find the report written by Cartwright…absolutely insane)
Based on the research presented by Dr. Cartwright in 1851, Black enslaved people who resisted enslavement by running away with hopes for freedom (typically called rascals and runaways) were deemed as ill. Cartwright created a name for this illness, ‘Drapetomania’ – the disease-causing Negroes to run away (PBS.org, nd). Cartwright explained in his report that the cause of this disease, in most cases, was a disease of the mind and was curable (PBS.org, nd). He suggested that if a slave master followed medical advice, did not allow Negroes to believe that they were equal to the slave master, did not allow the Negro basic comforts and necessities of life, and kept him/her in a position of submission as instructed in the scriptures Bible, then the Negro would not have a reason to flee because he would be “spell-bound” and unable to run away (PBS.org, nd). Cartwright stated that if the slave masters were not careful, the enslaved person may become rude and ungovernable, therefore, they should ensure that the enslaved person is fearful. Cartwright suggested, if one of them should be brave enough to attempt to run away, they should be beaten; typically known as “whipping the devil out of them” (PBS.org, nd). Have you ever heard an adult in your life use that term???
Dr. Cartwright also suggested that Black enslaved people who are treated kindly, clothed, and fed, separated into families with homes of their own while not allowed to be out at night, have visitors, or able to indulge in alcohol are easily managed, more manageable than any other race (PBS.org, nd). Could you imagine???
To add insult to injury, Cartwright came up with another mental illness diagnosis, specifically for the Black/African American enslaved people. This one was called Dysaethesia Aethiopica or hebetude of mind and obtuse sensibility of the body – a disease peculiar to Negroes, called by overseers, “Rascality” (PBS.org, nd). With this disease, Cartwright explained that enslaved people seem to be like a person who is half asleep, they are not aroused and struggled to stay awake, there were physical signs of lesions on the body, more prevalent among free Negroes when they lived in “clusters by themselves”, and found among enslaved people who tried to live like free Negroes by doing things such as exercising, eating healthy, dieting, etc. (PBS.org, nd). Cartwright characterized the person as being mischievous, “owing to the stupidness of mind and insensibility of the nerves induced by the disease”, they waste time and destroy everything they touch, they abuse the animals, ignore the rights of property, steal, and so on (PBS.org, nd). Dr. Cartwright continued to suggest that the behaviors immolated that of children, stating that those suffering from this disease needed to be governed in all that they did (Academic Support for Nursing Students, 2020). According to Cartwright, Dysaethesia Aethiopica was the “natural offspring of Negro liberty – the liberty to be idle, to wallow in filth, and to indulge in improper food and drinks” (Academic Support for Nursing Students, 2020; PBS.org, nd). Basically speaking, Dr. Cartwright informed the White communities that Black/African American enslaved people had to remain in the care of their “owners” because they would otherwise become ill and destructive.
To reiterate, Dysaethesia Aethiopica was a disease of the mind and body. Behaviors were characterized as symptoms that include careless movements, intentional mischief, the breaking, wasting, and destroying of things, and disruptive (Academic Support for Nursing Students, 2020).
Now, let us move into the 21st century…this is where you will begin to see what I see.
Today, there is a mental health disorder referred to in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSMV) called Oppositional Defiant Disorder (O.D.D.). Ironically, according to the Academic Support for Nursing Students (2020), O.D.D. is the “new” diagnosis for the insubordinate Black/African American person (I can see the correlation). Symptoms of this disorder include temper tantrums, argumentative, angry, defiant, vindictive, and resistance to authority, very similar to those symptoms of Dysaethesia Aethiopica (Academic Support for Nursing Students, 2020; American Academy of Child & Adolescent Psychiatry, 2019; Ballentine, 2019). Studies indicate that Black/African American children may be over-diagnosed with O.D.D. (Ballentine, 2019). Further studies indicate that Black/African American males are diagnosed at a disproportionately higher rate than their White counterparts (Academic Support for Nursing Students, 2020; Ballentine, 2019). Unfortunately, none of this is surprising.
Okay…I am going to stop right here, just for a second as I must interject a few more points. OMG! There is so much I want to share but I must try to make this as short as possible…this is crazy!
I would like to bring us back to generational trauma. Here is something else from our past that I believe is relevant to today.
Scientific racism (another piece of information I had no idea about) is an interesting one. What makes this interesting is the person who I find referenced when researching this “term", not only signed the Declaration of Independence, but he was also the founder of the first anti-slavery society in America and a leading mental health reformer. Dr. Benjamin Rush, the Father of American Psychiatry (remember, the organization that offered an apology letter this past January) and surprisingly (not really), the owner of a child slave who he eventually freed for compensation, described Negroes as “suffering from an affliction called Negritude – a mild form of leprosy with only one cure and that is to become white (Dickinson University, nd; University of Dayton, 2008; Plummer, 1970). Through his conflicting views, many were led to believe that darker skin was an illness that could be cured by simply lightening the skin, something that Dickinson University’s (nd) site mentioned Rush saw another scientist do when he poured muriatic acid on an African American man. The diagnosis leads the White community (and by osmosis, the Black/African American community) to believe darker skin was related to this disease. This insane diagnosis played a role in the pseudoscientific beliefs that justify racism, racial inferiority, and superiority.
More discriminating suggestions in psychology…
In 1895, after the Civil War, there was an increase in the number of Black/African Americans admitted into mental health hospitals (known as lunatic asylums). Dr. T.O. Powell, from Georgia, suggested that Black/African Americans were unable to manage once freed causing them to indulge in activities that encouraged insanity. What he did not consider was the individuals’ socioeconomic conditions, discrimination, and their response to violence (i.e., lynchings) (Umeh, 2019).
Lobotomy – removal of part of the brain, was popular for Black/African Americans between the 1930s and 60s. This was a standard practice when treating mental illness, brain dysfunction, urban violence, and inner-city uprisings – a reaction to systemic oppression, poverty, discrimination, and police brutality (Umeh, 2019).
Postpartum depression (PPD) is seen in 20% of all women but over 40% in Black/African American women (Umeh, 2019). Once again, social, and environmental circumstances are and were typically the cause, such as poverty, socioeconomic status, poor resources and access to healthcare, and single parenting.
These are just a few of many, and more horrendous examples of how psychiatry has and continues to play a major negative role in the Black/African American community.
We hear politicians talk about the needs of the country and how they will address the issues surrounding Black/African American communities, but we still find ourselves fighting for total freedom and equity. Umen (2019) shared that in 1983, one in two Black children lived in poverty in comparison to one in seven White children. Today, it is one in three Black children living in poverty compared to one in 10 White children.We know many of the factors associated with mental illness. We know that mental illness typically shows its ugly head by the time our children are 14 years of age. We realize that systemic discrimination, oppression, police brutality, mental illness, addiction, incarceration, and low-socioeconomic status, encourage mental illness in our children.
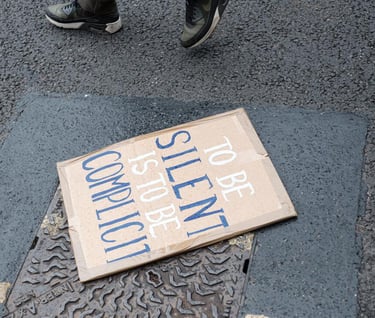
What do you do? How do you begin, as a community, as a race, to fight against a system --- a group of people that have worked so hard to keep you, an entire race of people, down?
The American Psychiatric Association, an organization that has had so much power over centuries, admits to deceiving, ignoring, and outright dismissing the Black/African American people. As the story goes, somewhere around 1843, the Eastern State Hospital’s (now known as APA) treatment system was changed and aligned with the racist and political policies taking place during that time (APA, 2021). Drapetomania was at the forefront of care leading doctors all over the country to believe that Black/African Americans who wanted freedom were mentally ill (APA, 2021). Over the years, until 2021, the APA “failed to act in Black Americans’ interest while White supremacists lynched Black people during the Reconstruction Era and Jim Crow segregation leading to Separate but Equal standards. The APA further failed to support Brown vs Board of Education and other major civil rights legislation that would have helped to improve social/psychological conditions for Black people” (APA, 2021).
It is 2021, the apology is here. The apparent changes are being made…so we are expected to believe. Now what? Where do we go from here?
Present-day trauma (PDT) is what I call the experiences of Black/African Americans today. We have experienced over 400 years of oppression and trauma and the beating continues. Our young people, particularly those in high crime and impoverished communities, experience stress similar to that of soldiers who have gone to war. Although their experiences may differ, our privileged youth experience present-day trauma as well. As soon as they turn on the television or jump on social media, there it is, all the violence and negative visuals one could ever imagine. It is a very frightening, stressful situation…daily.
As a therapist, I must also mention another side to this. It saddens me when I have clients who appear to have, what I call situational trauma or a temporary setback, and must receive a documented diagnosis for their insurance to flip the bill for a service they so desperately need. Labeling is a horrible thing for so many reasons…sadly, that is a whole nother topic. Without a diagnosis, stating that the person has a mental illness, we cannot bill insurance companies. Then we wonder why Black/African Americans do not trust the system. It is clearly not set up for us. Yes, White people get therapy and need a diagnosis too but when you check out the data, they are not the ones with the most discriminating diagnoses, the Black/African Americans are. I am all for helping anyone who needs assistance, especially the youth. I will always extend my hand and heart to mankind of all backgrounds. But the fact of the matter is that our White, Hispanic, Asian, or any other counterparts are not the majority of those being negatively impacted in this area. This is a real issue ya'll.
Honestly, I believe the presented factors are here to stay, just for a little while longer. In the meantime, and in between times, it is important for us as adults, parents/caretakers, teachers, and community leaders, to remember, to not look at one’s behavior and determine the reason for that behavior as being a mental health disease without considering the social or environmental aspects of one’s existence. This is especially common, from my experience, with Black/African American people…young and old. When addressing an issue surrounding the actions or behaviors of a Black/African American, it is most common to blame the individual and not the social or environmental circumstance that may be the cause of the action or behavior. Considering the history of psychiatry, it is no wonder we are where we are as a race. Thing is, now we know. It is time to do different and be different.
In this piece, we have explored the problem, we have come to understand the barriers, now we must face this battle head-on, as a community. I think it is time for us to stop putting our needs in the hands of others and work together to ensure the safety and well-being of ourselves, our families, our communities, and our race. If we have learned nothing else over this past year, we did learn that we are stronger together. We learned that we are more supportive and loving toward one another than we could have ever imagined. We learned that the jig is up and unlike what we have been brainwashed to believe, Black/African American people are not our own enemies.
Let’s rock!!!
Queendom rising!
References for your personal review:
Abrams, Z. (2020). Sounding the alarm on Black youth suicide. American Psychological Association. Retrieved from https://www.apa.org/news/apa/2020/black-youth-suicideAcademic
Support for Nursing Students. (2020). Influence of Drapetomania and Dysaethesia Aethiopica on pathologisation of Black resistance. Black resistance as illness. Retrieved from https://nursinganswers.net/essays/influence-of-drapetomania-and-dysaethesia-aethiopica-on-pathologisation-of-black-resistance.phpAmerican
Academy of Child & Adolescent Psychiatry. (2019). Oppositional Defiant Disorder. Retrieved from https://www.aacap.org/AACAP/Families_and_Youth/Facts_for_Families/FFF-Guide/Children-With-Oppositional-Defiant-Disorder-072.aspxAmerican
Psychiatric Association. 2021. APA’s apology to Black, Indigenous and people of color for its support of structural racism in psychiatry. American Psychological Association. Retrieved from https://www.psychiatry.org/newsroom/apa-apology-for-its-support-of-structural-racism-in-psychiatryAmerican
Psychiatry Association. (2021). Historical addendum to APA’s apology to Black, Indigenous and people of color for its support of structural racism in psychiatry. Retrieved from https://www.psychiatry.org/newsroom/historical-addendum-to-apa-apologyBallentine,
K. L. (2019). Understanding Racial Differences in Diagnosing ODD Versus ADHD Using Critical Race Theory. Families in Society: The Journal of Contemporary Social Services. doi: https://doi.org/10.1177/1044389419842765Bridge,
J. A., PhD., Horowitz, L. M., PhD., MPH, Fontanella, C. A., PhD, et al. (2018). Age-related racial disparity in suicide rates among US youths from 2001 through 2015, JAMA Pediatrics, 172(7), 697-699. doi: 10.1001/jamapediatrics.2018.0399
Dickinson University. (nd). Benjamin Rush. Retrieved from https://www.dickinson.edu/info/20043/about/3480/benjamin_rushLindsey,
M. A., Sheftall, A. H., Xiao, Y., and Joe, S. (2019). Trends of suicidal behaviors among high school students in the United States: 1991-2017. Pediatrics, 144(5). doi: https://doi.org/10.1542/peds.2019-1187PBS.org. (nd).
Diseases and peculiarities of the Negro race. Africans in America. Retrieved from https://www.pbs.org/wgbh/aia/part4/4h3106t.htmlPlummer, B. (1970).
Benjamin Rush and the Negro. American Journal of Psychiatry, 127(6). Retrieved from https://ajp.psychiatryonline.org/doi/pdf/10.1176/ajp.127.6.793Sibrava,
N. J., PhD., Bjornsson, A. S., PhD, Benitez, A. C. I. P., PhD., Moitra, E., PhD., Weisberg, R. B., PdD., and Keller, M. B., MD. (2019). Posttraumatic stress disorder in African American and Latino adults: Clinical course and the role of racial and ethnic discrimination. American Psychologist, 74(1), 101-116. doi: 10.1037/amp0000339Umeh, U. (2019).
Mental illness in Black community, 1700-2019: A short history. Retrieved from https://www.blackpast.org/african-american-history/mental-illness-in-black-community-1700-2019-a-short-history/
University of Dayton. (2008). An early history – African American Mental Health. Race, Health Care and the Law. Retrieved from https://academic.udayton.edu/health/01status/mental01.htm
